Who hasn't heard of the nose bob or the nose job? Cosmetic surgeons, rather more sedately, call it rhinoplasty. It's the most-requested procedure for the face, the one that can make the most dramatic difference on some faces and, unfortunately, also the one with the highest rate of post-op dissatisfaction (either because of over-expectations on the part of the patient or over-correction on the part of an ambitious surgeon, or because tricks by Mother Nature or due to constitutional factors can distort the intended result).
The first nasal surgeries are credited to the great Indian practitioner, Sushruta, in the 6th century B.C. In modern times, the development of nose correction procedures has closely paralleled the advancement of cosmetic surgery itself. In fact it was the nose bob that first made plastic surgery a household word. Until the early part of the 20th century, however, the surgical incisions were mostly placed outside the nose; today, they are placed inside the nose so that scars are not visible.
Additionally, techniques are far more refined today. While the earlier corrected noses had a "surgical look", today's new noses are more natural in appearance. The first rhinoplasty operations in recent times were directed at reducing the size of the nose; today, noses can be made smaller or larger, turned up, pushed back, have their nostrils thinned, their profiles made aquiline and much more.
Nose jobs may be requested for a number of different reasons :
- Congenital malformations including deviated septum, saddleback deformities, double humps etc.
- Aesthetic purposes such as refining a bulbous tip, trimming a long nose, narrowing down flared nostrils, etc.
- Reconstruction of the nose (or a part of it) which may be required following severe injury, an accident or cancer surgery.
The surgery therefore basically involves altering or restoring nose shape by one or more of three approaches :
- Removing underlying bone or cartilage
- Moving and reshaping this underlying structure
- Adding to it through the use of silastic implants. The skin is then re-draped over the new contours.
The procedure is essentially akin to raising or lowering the central support of a tent, thus altering its external appearance.
- Pre-Surgery Preparation
Perhaps no other cosmetic procedure calls for as much planning, aesthetic judgement and careful preparation as nasal surgery.
At your pre-op clinic visits, your surgeon if he's a skilled and ethical practitioner will lead you through an extended amount of groundwork : discussions, photograph-taking, detailed examinations of not only your nasal profiles but also of the other features of your face. His efforts will be directed at not just correcting the obvious defect in the nose or refining and redefining its shape, but also in ensuring that taken in conjunction with the other features of your face the final look will be balanced and pleasing to the eye. One reason for the "something's missing" look in the results of earlier rhinoplasty was, that, while noses were corrected, chins were left intact; today, we know that many patients undergoing nasal surgery can also benefit from having their chins altered. (For instance, those with large noses unfortunately, but commonly, have weak or small chins).
Sometimes alterations in the area of the upper lip which is contiguous with the nose are also required along with the nasal correction.
Even in planning the correction of the nose alone, the surgeon must consider the fine aesthetic balance that he needs to maintain among its various aspects : the bridge, the tip, the nostrils, the root of the nose (i.e. the area where the nose joins the forehead). For this reason, he will need to take, and to show you, professional photographs which should include the full face, two profiles, a smiling view and a basal or "worm's eye-view" taken from a low angle.
Your intended surgeon will try to determine your motivation for altering the shape or size of your nose, and whether your expectations are realistic. This is the time you must express yourself fully so that he can tell you not only what is possible in your case, but also what is not. He can show you this more precisely by inking in alterations on your photographs or, more commonly today, with "computer imaging" which allows you to electronically preview the expected post-op results. But remember, all these are approximations, there are no guarantees. So, too, with the 'before' and 'after' pictures of his previous patients that a surgeon might show you: they give you a sense of his aesthetics, and of what is possible in nose correction surgery, but they won't tell you the exact result you can expect on your own nose.
Some expectations are clearly unrealistic : to expect a surgeon to alter a large bulbous, thick-skinned nose into a finely-chiselled feature, for instance. An extent of improvement can definitely be expected, but not a total transformation, and as the patient you should know this before the operation, not after.
Though standardized concepts of the "ideal nose profile" do exist, the wise surgeon will use this only as a general aesthetic guide, and not try to make every patient conform to the mould; in the end, it is the harmonizing of the individual patient's features that will make for the "best" result.
The pre-op examinations will include inspection of the intra-nasal area, especially if a nasal obstruction or inside growth exists.
Also important is checking the thickness of the nasal skin. Thick, rigid skin does not drape as well over the re-modelled nose as fine textured skin (the rhinoplasty surgeon's delight, especially if it accompanies a long, thin nose).
At what age can you have your nose done? Most cosmetic surgeons agree that nasal surgery can be undertaken once the nose has attained about 90 per cent of its adult size, at about 13 years for girls, and 15 for boys. (The exception, of course, is the correction of a serious birth defect which interferes with breathing and may stunt the development of the lungs and needs to be tackled urgently). What is more important is that an adolescent should have attained the emotional maturity necessary to handle the implications, and especially the aftermath, of the surgery. In fact, the `cope-able' adolescent patient is often the best candidate for nasal surgery; greater prudence on the part of the surgeon is called for, in undertaking corrective surgery in the older patient in whom the skin is also less elastic and will not settle down as easily into its new shape. On the other hand, this does not mean that 50 or even 60 is "too late" to have nasal surgery. Only, healing will take slightly longer.
- Operation
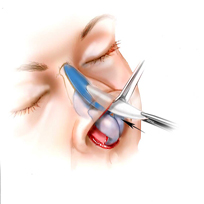
Either local or general anaesthesia can be used, coupled with an intravenous sedative. An adequately-sedated patient is likely to experience less bleeding during the surgery than a nervous one. The surgery takes from an hour to two hours, depending on what needs to be done. Different deformities require different approaches and procedures; most surgeons, however, find it useful to follow an "order of procedure", especially in treating the most common nasal deformity, the nose with a hump which may be too long or too large and generally accompanied by some kind of abnormality of the nasal tip.
Often, correcting one type of deformity requires accompanying alterations to be made in one or more other nasal features in order to maintain a balanced nasal profile. Thus, if the contour of the bridge is corrected, it may be necessary, to also alter the tip surgically, so that it fits well over the new bridge; to neglect to do this may bring on what is known as a "polly-tip" deformity.
In most rhinoplasty procedures today, the incisions are placed inside the nose. There are exceptions, such as surgery to reduce the flare of the nostrils, in which case the incisions are made in the groove of each nostril. These are rarely visible and, even they fade with time.
- Post-Operative Care
When the surgery is complete, a Plaster of Paris or a metal splint is applied to the nose to keep the new structure in position and to limit swelling; it stays on for five to seven days. In some nasal procedures, a small amount of surgical packing is inserted inside the nose at the end of the operation and kept in for the first 24 Hours. It helps to control post-operative bleeding, and-though it is a source of annoyance to the patient-the longer it is kept in, the easier it is to remove, without disturbing the healing tissues.
Medications and antibiotics are routinely given to control the pain, infection risk and inflammation. Bleeding is less, and healing faster, if the patient is left undisturbed.
On average, you'll need to stay in the hospital for about 6 hours. In the early post-operative period, you will be advised to sleep with your head raised, so as to minimize oozing. Ice compresses may be placed over your eyes. They chiefly have a soothing effect: they do not lessen the swelling and discoloration that appear around the eyelids, nor hasten their disappearance.
You will also be asked to observe a whole set of cautionary do's and don'ts, all aimed at preventing loosening of the splint, avoiding distortion of the newly-created structure and promoting healing. They include:
- Stay on a liquid/soft diet during the first two days after surgery to minimize mastication (which could pull on the operated nose).
- In the initial period, breathe through your mouth until the nasal passages clear sufficiently to permit breathing through the nose.
- For about a week after the splint has been removed, avoid blowing your nose: it could provoke hemorrhage as well as pain.
- When you sneeze, keep your mouth wide open, exhale as much air out of your lungs as you can before you actually sneeze to reduce the intensity of the sneeze.
- After the splint has been removed, clean your nostrils three to four times a day with cotton buds, and apply cold cream or Vaseline inside the nose to soften the blood clots or crusts.
- Avoid compressing the nostrils, playing around with the new shape of your nose or inserting objects inside the nose: this could bring on trauma as well as scarring.
Expect swelling and discoloration around the eyelids to continue for seven to ten days. Sometimes the whites of the eyeballs appear red due to the blood, that has escaped from the nasal area into the eyeballs. This is known as a sub-conjunctival hemorrhage and will also spontaneously disappear, by around the tenth day.
Swelling around the nose takes a much longer time to settle down. About 90% of it will have disappeared within a fortnight but a minimal amount of swelling may persist even upto a year, especially in the area above the tip of the nose or at the root of the nose (i.e. the area where the nose joins the forehead). The older the patient, and the greater the amount of reduction in nose size, the longer it will take for the swelling to subside. This residual swelling is not conspicuous; it exists more as a feeling of tissue firmness.
The tissues lining the inside of the nose will also be swollen post-operatively, resulting in some degree of nasal blockage and therefore mildly obstructed breathing for about three months.
You will definitely need to take time off from work for two to three weeks to avoid exposing your nose to external hazards. You'll also be instructed not to over-expose your face to the sun for the first few months since its strong rays can burn the skin of your nose at a time when the blood supply has not completely returned to normal.
Although the nasal chiselling performed at the time of the surgery takes about six weeks to completely heal, you can get back to routine activities in about two to three weeks. However, you'll need to avoid contact sports such as football and wrestling because of the risk of dislocating the healing nasal bones.
- Risks and Complications
- Post-operative bleeding : Hemorrhage is an infrequent complication of rhinoplasty, is usually not severe and is easily controlled by removing clots and re-packing of the nose with gauze. Bleeding is a more likely occurrence if a procedure involving the nasal septum (the partition between the two sides of the nose) has been done. It can also be provoked by picking the nose post-operatively or by exertion.
- Infection : If hematoma (collection of blood clots) has been carefully avoided by the surgeon, and if he has removed fragments of bone or cartilage at the completion of the procedure, infection is unlikely. The rare abscess that does occur is tackled by its incision and drainage and with antibiotics.
- Malfunctioning of the nose (that is, breathing difficulties, may result from faulty surgery, such as destruction of part of the musculature of the nose in an effort to thin the nose, or through excessive removal of the cartilage (which is the framework upon which the muscles rest and act). Since the nose is not just a static facial "feature" but an organ of breathing, it cannot simply be shaped at will on the operating table; the surgeon must take great care to preserve the dynamics of its normal functioning. Excessive removal of the cartilage of the nose-tip may result in a 'pinched-tip', which may not become apparent until two or three years after the surgery.
- Drooping of the tip : Due to the dressings as well as the initial swelling, the tip of the nose is temporarily elevated in the immediate post-surgery period; as the swelling subsides, the tip resumes its position,. But the patient often interprets this as a downward drooping of the tip. The surgeon's assurance is needed at this stage so that the patient knows that the early droop is in fact intentional. At times, however, drooping of the nose tip may in fact be caused by poor surgical judgement or execution, resulting in over-correction. This can undermine an otherwise satisfactory outcome.
- Poor Healing : Some of the most unfortunate effects of nasal surgery result from the fact that the process of healing is so unpredictable. Excessive scar tissue may form inside causing tissues to be pulled into abnormal positions. Some patients scar badly. (Darker skins are more prone to poor scarring). Poor blood supply can cause temporary or permanent discoloration of the skin. In thin-skinned persons, this can result in dark rings under the eyes. If there is abnormal absorption or re-setting of the nasal bones at the places where they have been cut, the new nasal framework can collapse. Much of the healing process is controlled by Nature, and sometimes Nature does play cruel tricks.
- Patient dissatisfaction : This is perhaps the main risk in nasal correction: that the patient is unhappy with the result. Most frequently it arises from a combination of over-expectations on the part of the patient and over-ambition on the part of the surgeon. When an effort has been made to accomplish more than the local tissues will permit, dissatisfaction is inevitable. It is often better to settle for less-than-perfect results rather than to reach for the unattainable and be foredoomed to failure. To a lesser degree, temporary dissatisfaction may be caused by minor irregularities in the contours of the new nose. Generally these are not obvious to the rest of the world, only to the patient and to the surgeon and that only on palpiation of the area. Many of these irregularities settle down in time, generally within three to six months. In fact, the virtue most demanded by nasal surgery is patience. If you expect to see your "new nose" immediately after the dressing is removed, you're being far too precipitate,. The nose is notorious for taking the longest time to settle into its new shape. One famous cosmetic surgeon has described the "settling-in" process as akin to the development of a Polaroid picture: it gets better and brighter all the time. Although the new nose is 90 percent "there" within about three months, you might need to wait upto eight to eighteen months, to see the absolutely final result. You'll know your plastic surgeon has done a poor job if you hear comments such as "Have you done something to your nose?" You'll know he's done a great job if people comment that "Your face is looking better", but cannot exactly say Why : that's something only you and your surgeon should be able to tell !